Administrative Simplification
simplifying healthcare
Administrative costs pose significant burden for all commercial/government health and workers’ compensation organizations, both in dollars and in time. Many “back-office” processes that offer no competitive advantage are ripe for centralizing. AAPAN and its members actively explore and develop solutions that bring about operational efficiency and reduce costly burden.
AAPAN is currently establishing a credentialing alliance that would be available to members and non-members alike. We are also exploring strategies for achieving efficiencies by streamlining non-proprietary data collection, network development, provider directory information accuracy and more. The association is a leader in simplifying healthcare administration.
Advocacy
AAPAN advocates at the federal and state level to ensure that policymakers understand the value our Commercial/ Government Health and Workers’ Compensation members bring to healthcare.
Administrative Simplification
AAPAN drives efficiencies in Commercial Health and Workers’ Compensation to improve the healthcare experience for both patients and injured workers.
Collaboration
AAPAN unites Commercial/Government Health and Workers’ Compensation organizations fostering open dialogue in a unique, collaborative atmosphere.
National Credentialing Alliance
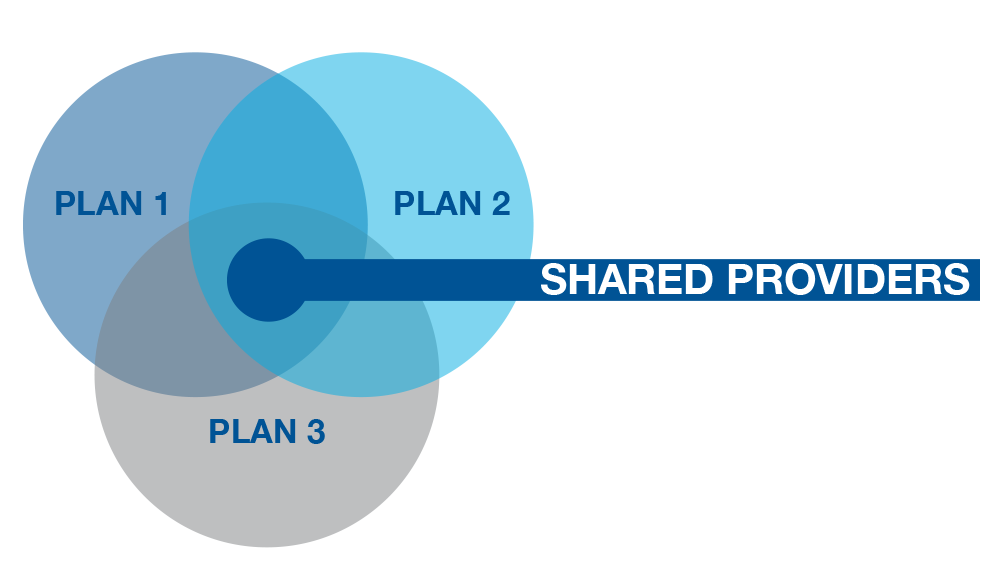
The alliance model works by aligning the credentialing dates of providers that participate in multiple plan networks, drives out redundant primary source verification costs for those plans and reduces administrative workload.
Why did AAPAN Creating a Credentialing Alliance?
Credentialing is a necessary, redundant task that every health care organization, including payers, networks and providers, must deal with. The American Association of Payers, Administrators and Networks (AAPAN)—a national not-for-profit trade association for payers, administrators, networks and care management organizations operating in the commercial/government health and workers’ compensation markets—is developing a solution to streamline the process while reducing cost, redundancy and the administrative burden.
How It Differs from the Current Process?
Today a provider that is participating in five different networks will go through the credentialing process five different times over a three-year period. With the AAPAN Credentialing Alliance, all those credentialing dates are aligned. The provider only goes through the credentialing process once and the cost is split between the five networks. Alliance members benefit from a significant reduction of cost, and providers benefit with a reduction of administrative workload.
Why Should Your Organization Care?
Unfortunately, we have witnessed an uptick in legislation—for example in Oregon and Washington—that streamlines credentialing to reduce the burden for providers. This process is creating a significant cost and burden to networks. There are other states that have implemented centralized Medicaid network credentialing, at much higher fees, with hopes of expanding to state commercial networks in the future. Other state introduced legislation has failed but time is running out for industry control.
In 2013, the State of Oregon passed legislation creating the Oregon Common Credentialing Program through the oversight of the Oregon Health Authority. The program was intended to simplify provider credentialing and was aimed at reducing costs and administrative burdens by eliminating duplication and centralizing data collection. In an opinion piece in the Morning Consult, it was noted that a credentialing alliance created by an AAPAN affiliate organization was significantly lower in cost than the state’s offering.
Fortunately, the state suspended the legislatively mandated provider credentialing program before launch, but it continues to be a consideration for many states. If we do not come together as an industry to create a solution, the government will.
Common Questions and Answers About the Credentialing Alliance
Does my organization need to pay to complete initial credentialing files through the Credentialing Alliance to join?
No. Your providers are imported via a simple .csv file where they will be reviewed and aligned based on your last credentialing approval date.
Is there a limit to the number of organizations that can share in the recredentialing fee?
No. The recredentialing fee can be divided by as many Credentialing Alliance members that share that provider.
When providers join our organization, we need them credentialed within a month. Is this possible with the Credentialing Alliance?
Yes. The average turnaround time (TAT) for completing initial files is five business days. The Credentialing Alliance TAT is calculated from the time a current/valid application is obtained and the file is completed – the clock does not stop if outreach is required.
How quick can the implementation process be completed?
From the Credentialing Alliance perspective, following the execution of documents, the time required for implementation is mainly reliant on the volume of providers being imported and compliance with the implementation template and data formatting.
Our client relationships require that all processing take place onshore. What is the additional fee for not using offshore resources?
All Credentialing Alliance services are performed onshore, no additional fee is required.
My organization considers our list of participating providers proprietary. Will other Credentialing Alliance member organizations be able to access our provider data?
No. The Credentialing Alliance is very committed to maintaining confidentiality and understands the proprietary nature of provider data. Each Credentialing Alliance Member can only access their own data.
Are credentialing activities completed in compliance with NCQA standards?
Yes. The Credentialing Alliance’s CVO partner just completed their most recent audit and continues to be NCQA Certified in all CVO categories.
Is it possible to obtain an estimate of the overlap/cost savings opportunity with the Credentialing Alliance?
Yes. All that is needed is a fully executed non-disclosure agreement and submission of a spreadsheet including provider names and NPI numbers.
Does the Credentialing Alliance offer access to credentialing related services other than primary source verification?
Yes. Currently in addition to CVO/PSV services, ongoing sanction monitoring and expirable management services are available. These services are also offered using the Credentialing Alliance shared pricing model.
Contact Carol Kurtz at (707) 372-1330 to get more information on joining the AAPAN Credentialing Alliance today.

